Imagine this: You’re in the middle of a bustling hospital, the air thick with the scent of antiseptic and the constant hum of activity. A patient is rushed in, pale and weak, clutching their abdomen in pain. Their vital signs are plummeting, and a dark, bloody discharge stains their sheets. This scene, unfortunately, isn’t a rare occurrence. Gastrointestinal (GI) bleeding, a serious condition where blood leaks from the digestive tract, can manifest in a variety of ways, causing significant distress and even life-threatening complications.
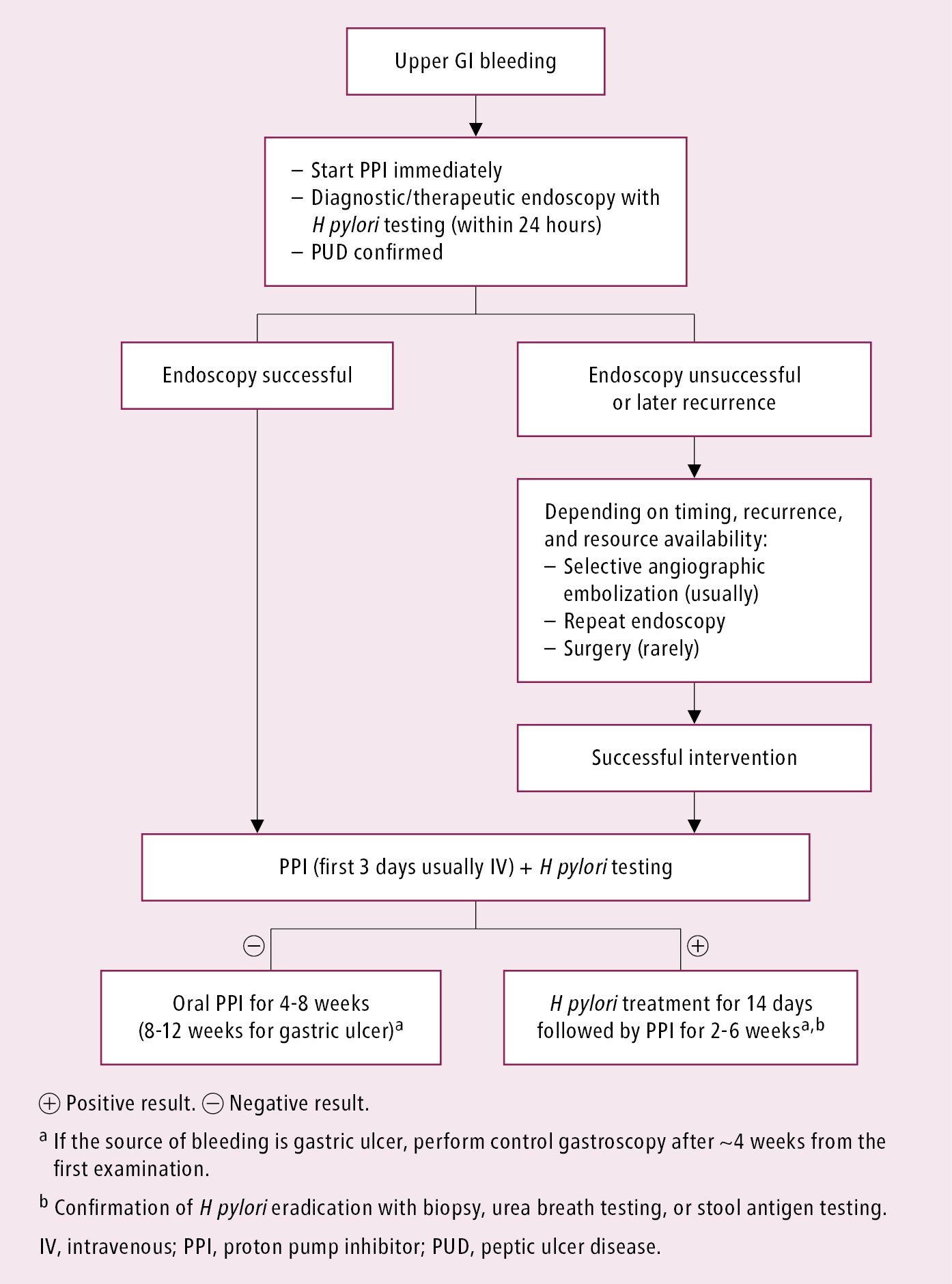
Image: diamondnewschurch.blogspot.com
As nurses, we play a critical role in identifying, assessing, and managing these patients. Understanding the underlying diagnoses associated with GI bleeding is crucial for providing safe and effective care. This article delves into the complex world of nursing diagnoses related to GI bleeding, equipping you with the knowledge and tools to effectively navigate this challenging area of practice.
The Foundation of Nursing Diagnoses: A Framework for Understanding GI Bleeding
At the heart of nursing practice lies the concept of nursing diagnoses. These are clinical judgments about an individual’s response to an actual or potential health problem that a nurse is licensed and competent to treat. They serve as a blueprint for planning and implementing individualized care, focusing on the patient’s unique needs and vulnerabilities.
When dealing with GI bleeding, nurses must identify and prioritize relevant nursing diagnoses, carefully considering factors such as:
- The patient’s age and overall health: Elderly individuals, those with underlying medical conditions, and patients on certain medications may be at higher risk for GI bleeding.
- The location and severity of the bleeding: Bleeding from the upper GI tract (esophagus, stomach, duodenum) often presents differently from lower GI bleeding (small intestine, colon, rectum).
- The cause of the bleeding: A variety of factors can contribute to GI bleeding, including ulcers, cancer, gastritis, inflammation, and certain medications.
- The patient’s specific symptoms: Nausea, vomiting, abdominal pain, fatigue, and changes in stool color can all be indicative of GI bleeding.
Navigating the Landscape: Common Nursing Diagnoses in GI Bleeding
Here are some key nursing diagnoses commonly associated with GI bleeding:
- Ineffective Tissue Perfusion: This diagnosis reflects the potential for inadequate blood flow to vital organs due to blood loss. Monitoring vital signs, assessing peripheral perfusion, and administering fluids are essential interventions.
- Acute Pain: GI bleeding can be accompanied by intense pain, requiring prompt pain management strategies.
- Deficient Fluid Volume: Blood loss can lead to dehydration and electrolyte imbalances. Ensuring adequate fluid replacement is crucial.
- Risk for Impaired Gas Exchange: Severe blood loss can compromise oxygen transport, making respiratory monitoring and interventions critical.
- Risk for Injury: Patients with GI bleeding may be at increased risk for falls or other injuries due to weakness or altered mental status.
- Risk for Infection: Open wounds or invasive procedures may elevate the risk of infection.
Tailoring the Approach: Individualized Care Planning
The individualized care plan is the cornerstone of effective nursing practice in GI bleeding. This plan must be tailored to the specific needs of each patient, taking into account their unique presentation, underlying conditions, and potential complications.
- Comprehensive Assessment: A thorough assessment is the foundation of care. This includes a detailed history, physical examination, and review of laboratory and diagnostic tests.
- Prioritization of Needs: Identify the most pressing nursing diagnoses and develop interventions to address them.
- Collaboration with the Team: Work closely with physicians, pharmacists, and other healthcare professionals to ensure coordinated care.
- Patient Education: Educate patients about their condition, treatment plan, and ways to prevent future complications.
- Continuous Monitoring: Regularly monitor vital signs, assess symptoms, and adjust interventions as needed.

Image: thestudycorp.com
Beyond the Basics: A Deeper Look at Nursing Considerations
Beyond the immediate care needs, there are several key nursing considerations that can significantly influence the course of treatment and recovery for patients with GI bleeding:
- Medication Management: Nurses play a vital role in administering medications, monitoring for side effects, and ensuring patient compliance.
- Nutritional Support: Proper nutrition is crucial for healing. Nurses may be involved in providing nutritional counseling, administering fluids, and monitoring for any nutritional deficiencies.
- Psychosocial Support: GI bleeding can be a stressful and emotional experience. Providing emotional support, answering questions, and addressing fears can make a significant difference.
- Discharge Planning: Nurses are instrumental in preparing patients for discharge, providing education on wound care, medication management, and follow-up appointments.
Empowering the Caregiver: Actionable Tips for Nurses
Here are some practical tips to enhance your nursing practice in the management of GI bleeding:
- Stay Up-to-Date: Continue your education to remain abreast of the latest advancements in the diagnosis and treatment of GI bleeding.
- Develop Strong Assessment Skills: Refine your ability to assess patients effectively, considering both physical and psychological factors.
- Cultivate Effective Communication: Communicate clearly and concisely with patients, families, and other healthcare professionals.
- Collaborate and Advocate: Work effectively with the interdisciplinary team to provide comprehensive care and advocate for your patients’ needs.
Nursing Diagnosis Related To Gi Bleeding
https://youtube.com/watch?v=YxDHv8AZHbI
The Guiding Light of Nursing: Conclusion
Managing GI bleeding is a complex and challenging task. As nurses, we play an essential role in identifying, assessing, and intervening on behalf of these patients. By mastering the concepts of nursing diagnoses, applying individualized care plans, and embracing ongoing professional development, we can provide compassionate and effective care, helping patients navigate this challenging health journey toward a brighter future.
If you have further questions or want to explore more in-depth information about nursing diagnosis related to GI bleeding, consider consulting with specialized resources, attending relevant conferences, or connecting with experienced colleagues in the field.






