Have you ever felt a persistent cloud of sadness hanging over you, making it difficult to enjoy the things you once loved? This is a common experience, and it may be a sign of depression, a serious mental health condition that affects millions of people worldwide. As nurses, we play a crucial role in providing compassionate care and support to individuals struggling with depression. A well-structured nursing care plan acts as a roadmap, guiding us in providing the best possible care for our patients.

Image: www.pinterest.com
This comprehensive article will delve into a sample nursing care plan for depression, outlining the key components that nurses utilize to provide holistic and effective care. From assessing the severity of depression to implementing evidence-based interventions, we will explore the essential aspects of a successful care plan. It’s important to note that this sample care plan is meant to be a guideline, and each individual’s needs may vary. We will discuss the diverse factors that impact depression, such as individual experiences, cultural background, and socioeconomic circumstances, ensuring a personalized approach to care.
Understanding Depression: A Complex Condition
Depression is not simply a passing mood; it’s a complex mental health condition characterized by persistent sadness, loss of interest, and feelings of hopelessness. It can affect a person’s thoughts, emotions, behavior, and physical health. Understanding the multifaceted nature of depression is crucial for developing a comprehensive nursing care plan.
Types of Depression
While we typically think of depression as a single entity, there are different subtypes, each with specific characteristics:
- Major Depressive Disorder (MDD): Involves persistent sadness, loss of interest, and other symptoms that impair functioning. This is the most common type of depression.
- Persistent Depressive Disorder (Dysthymia): A milder but longer-lasting form, lasting at least two years, characterized by low-grade depression with less intense symptoms.
- Seasonal Affective Disorder (SAD): A type of depression triggered by changes in seasons, usually during the shorter days of fall and winter.
- Bipolar Disorder: A condition involving extreme mood swings, cycling between manic or hypomanic periods and depressive episodes.
- Perinatal Depression: A depressive episode that occurs during pregnancy or the first year after childbirth.
Causes of Depression
The exact causes of depression are not fully understood, but research suggests a complex interplay of biological, psychological, and social factors. These include:
- Genetics: Family history of depression increases the risk.
- Neurochemical Imbalances: Differences in neurotransmitter levels in the brain, particularly serotonin, norepinephrine, and dopamine.
- Stressful Life Events: Loss of a loved one, financial difficulties, relationship problems, or major life changes.
- Chronic Medical Conditions: Certain illnesses like diabetes, heart disease, or cancer can contribute to depression.
- Substance Abuse: Alcohol or drug abuse can worsen depression or even trigger it.
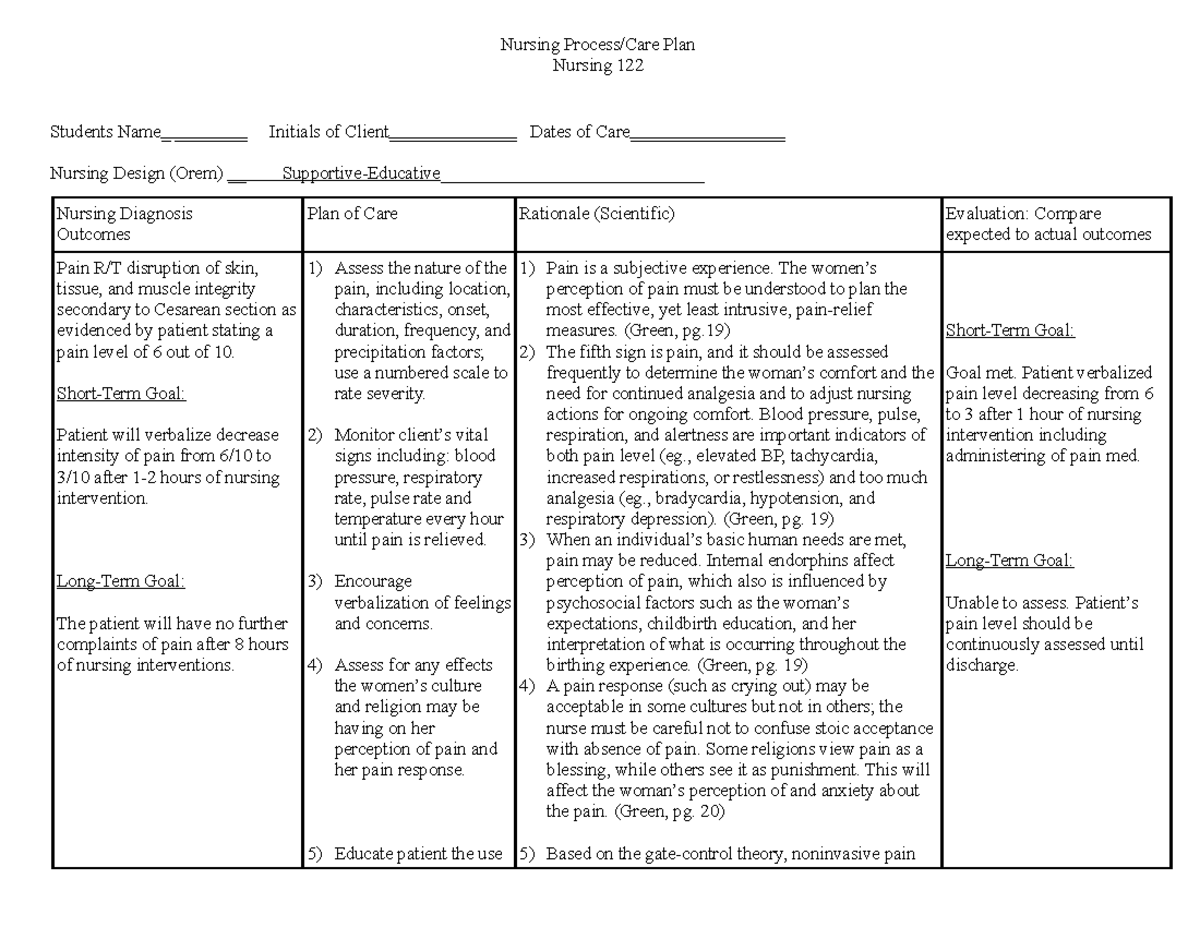
Image: fity.club
Assessing Depression: The First Step in Care
The nursing care plan for depression begins with a comprehensive assessment of the patient’s symptoms and overall well-being. This thorough evaluation helps identify the severity of depression, assess potential risk factors, and determine the most appropriate interventions. Here’s what the assessment typically involves:
1. Gathering Information
- Patient History: Reviewing the patient’s medical history, including any previous diagnoses of depression or other mental health conditions, medication history, and family history of mental illness.
- Physical Assessment: Assessing the patient’s physical health, checking for any underlying medical conditions that may contribute to depression.
- Mental Status Examination (MSE): Evaluating the patient’s mood, affect, thought processes, and behavior to assess the severity of depression.
- Psychosocial Assessment: Exploring the patient’s social support system, coping mechanisms, and stressors in their life.
2. Utilizing Assessment Tools
Nurses often use standardized assessment tools to measure the severity of depression and track progress over time. Some common tools include:
- Beck Depression Inventory (BDI): A self-report questionnaire that measures the severity of depressive symptoms.
- Hamilton Depression Rating Scale (HAM-D): A clinician-administered scale that assesses the severity of depression in a more comprehensive manner.
- Patient Health Questionnaire (PHQ-9): A widely used tool that screens for depressive symptoms.
3. Identifying Risk Factors
During the assessment, nurses are vigilant in identifying potential risk factors that may increase the severity of depression or the risk of suicidal thoughts or behaviors. These risk factors may include:
- History of Suicide Attempts: Past attempts increase the likelihood of future attempts.
- Family History of Suicide: A family history of suicide increases the risk.
- Substance Abuse: Alcohol or drug abuse can contribute to suicidal thoughts.
- Hopelessness and Feeling Overwhelmed: These feelings can magnify suicidal ideation.
- Access to Lethal Means: Access to firearms or other means of self-harm can increase the risk of suicide.
Developing a Nursing Care Plan for Depression
Once the assessment is complete, nurses work collaboratively with the patient, their family, and other healthcare professionals to develop an individualized nursing care plan. This plan outlines specific goals, interventions, and expected outcomes for the patient. Here’s a breakdown of the key components of a sample care plan:
1. Defining Goals
The goals of the nursing care plan are tailored to the individual patient’s needs and may include:
- Symptom Management: Reducing the severity of depressive symptoms, such as sadness, loss of interest, and sleep disturbances.
- Improved Functioning: Enhancing the patient’s ability to participate in daily activities, work, and social interactions.
- Increased Coping Skills: Teaching the patient healthy coping mechanisms to manage stress and emotions.
- Enhanced Self-Esteem: Promoting a positive self-image and helping the patient feel more confident in themselves.
- Suicide Prevention: Reducing the risk of suicidal thoughts and behaviors.
2. Implementing Interventions
The nursing care plan includes a range of evidence-based interventions that address the specific needs of the patient. These interventions can be pharmacological, psychological, or social in nature, and often involve a combination of approaches.
- Pharmacological Interventions: Prescribing antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs), to regulate neurotransmitter levels in the brain.
- Psychological Interventions: Providing psychotherapy, such as cognitive behavioral therapy (CBT) or interpersonal therapy (IPT), to help patients identify and change negative thought patterns and behaviors.
- Social Interventions: Encouraging the patient to engage in social activities, build a support system, and connect with others.
- Lifestyle Modifications: Recommending lifestyle changes that promote mental and physical health, such as regular exercise, a balanced diet, and adequate sleep.
- Electroconvulsive Therapy (ECT): A procedure that involves inducing a brief seizure using electrical impulses, which can be effective for severe depression that hasn’t responded to other treatments.
3. Monitoring Progress and Evaluating Outcomes
Nurses regularly assess the patient’s progress against the goals outlined in the care plan. This ongoing monitoring involves:
- Assessing Symptoms: Observing for changes in the patient’s mood, behavior, and overall well-being.
- Evaluating Medications: Monitoring for side effects and effectiveness of prescribed medications.
- Tracking Therapy Sessions: Reviewing the patient’s progress in therapy and discussing any challenges they may be facing.
- Evaluating the Patient’s Quality of Life: Assessing the patient’s satisfaction with their overall well-being and level of functioning.
4. Providing Education and Support
Nurses play a crucial role in educating patients and their families about depression and its management. This education covers:
- Understanding Depression: Explaining the symptoms, causes, and treatment options for depression.
- Medication Information: Providing detailed instructions about prescribed medications, including dosage, potential side effects, and how to manage them.
- Therapy Strategies: Discussing the goals and techniques of psychotherapy and how the patient can actively participate in therapy.
- Self-Care Strategies: Encouraging healthy lifestyle practices, such as regular exercise, a healthy diet, and getting enough sleep.
- Coping Skills: Teaching the patient effective coping mechanisms for dealing with stress, anxiety, and other challenges.
- Support Resources: Connecting patients with local mental health support groups, organizations, and hotlines.
Navigating Ethical Considerations in Depression Care
As nurses, we uphold ethical principles that guide our interactions with patients. When providing care for individuals with depression, specific ethical concerns arise, requiring careful consideration:
1. Privacy and Confidentiality:
Information shared by patients with depression is highly sensitive. Nurses must maintain absolute confidentiality and respect their privacy. This extends to all aspects of care, including conversations, records, and sharing information with other healthcare professionals.
2. Informed Consent:
Before implementing any interventions, including medications or therapy, patients must provide informed consent. This means they have a clear understanding of the procedure, benefits, risks, and alternatives.
3. Autonomy:
Patients have the right to make decisions about their care, even if these decisions differ from the nurse’s recommendations. Nurses must respect their autonomy and empower them to make choices that align with their values.
4. Duty to Warn:
In situations where a patient expresses suicidal thoughts or has a plan for self-harm, nurses have a duty to warn the appropriate authorities. This delicate balance involves respecting the patient’s privacy while ensuring their safety.
5. Non-Judgemental Approach:
Nurses must approach patients with depression without judgment. They should avoid stigmatizing language and create a safe and supportive environment where patients feel comfortable expressing their experiences.
Sample Nursing Care Plan For Depression
Conclusion: Empowering Recovery with Compassionate Care
Providing compassionate and effective care for individuals with depression is a complex but rewarding endeavor. A well-structured nursing care plan, encompassing assessment, intervention, monitoring, and support, can empower patients on their journey toward recovery. By understanding the multifaceted nature of depression, utilizing evidence-based practices, and upholding ethical principles, nurses play a critical role in improving the lives of those affected by this debilitating condition. Remember, every individual with depression has a unique story, and our job as nurses is to listen, care, and guide them on their path to healing. Continue to explore resources, engage in research, and advocate for improved mental health services. We can collectively work towards a world where individuals with depression receive the care, support, and acceptance they deserve.






